Osteoporosis is a bone disease that approaches stealthily. For a long time there are no symptoms, then at some stage you experience unexpected back pain. However, medical professionals often only identify the disease due to a rapid shrinking in size or a bone fracture. However, the sooner you know about your bone density, the sooner you can react with measures that are healthy for your bones, if these are required. But how can osteoporosis be prevented and how can it be detected? We will clarify this and more in this article.
What is osteoporosis?
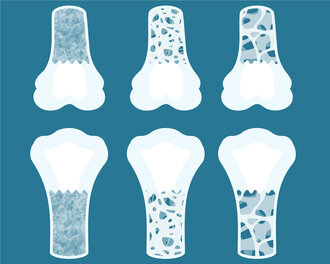
Osteoporosis is a bone disease in which the density, quality and firmness of the bone is reduced. A certain loss of bone density is normal and even natural from a certain age. However, in osteoporosis (= bone loss) and its precursor, osteopenia, the bone substance degrades to an increased extent. Bones lose density and stability – the risk of bone fracture increases.
Osteoporosis does not only strike in the elderly. In juvenile osteoporosis, bone density is already reduced in childhood and adolescence. Possible causes include calcium and/or vitamin D deficiency and a low-exercise lifestyle.
Osteopenia or osteoporosis? Course of osteoporosis:
Simply put, the term osteopenia describes an intermediate stage between healthy bone and osteoporosis. Even at this stage, bone density is lower compared to normal bone, but it is not yet osteoporosis. Important to know: Osteopenia does not necessarily have to end in osteoporosis.
Bone density is usually determined by special X-ray procedures on the spine and hip. If your bone density is too low for your age, you either have osteopenia or osteoporosis – depending on how severe the deviation is. Then there is a need for action.
What is meant by manifest osteoporosis?
Manifest osteoporosis is when at least one osteoporosis-related bone fracture has already occurred as a visible consequence of osteoporosis.
Osteoporosis: A hardly noticeable disease with significant consequences in old age
It is already one of the most common diseases in Central Europe. Around 3.5 million British people are already affected by osteoporosis. However, since osteoporosis primarily occurs in advanced age, young people are often relatively casual about the disease. This is a fatal error, because from the age of 35 onwards, bone mass is already decreasing, at first very slowly, but then – especially in the absence of measures with regard to sports and nutrition – with increasing speed.
Osteoporosis signs & symptoms: How can bone loss be detected early?
You cannot feel osteoporosis or quickly identify it yourself based on other symptoms. However, the loss of bone mass inevitably occurs and can be detected early by special bone density measurements and intercepted to a certain degree. As so often, genes also play a role. You should be particularly vigilant if your own parents are affected – that is, if they have a significantly hunched back, have shrunk quite a bit in size or have already suffered a femoral neck fracture.
Menopause and bone density
For women, the loss of bone density increases dramatically at around the age of 50, because the rate of bone degradation accelerates during the menopause. Why? The production of female sex hormones in the ovaries decreases and a significant impulse that inhibits bone degradation disappears with the oestrogens.
If the age-related decrease in bone density in younger years is on average 1.5% annually, this increases to up to 5% after menopause. It is a very good idea to have a bone density scan during this time. This is because, if osteoporosis or the precursor stage osteopenia is detected in a timely manner, it can still be counteracted.
Does osteoporosis only affect women or are men affected too?
Osteoporosis is definitely not simply a “women’s disease”. Men are affected much more frequently than is generally assumed. In addition to heredity, the “typically male” lifestyle is also associated with some risk factors. Osteoporosis in men can be attributed to unhealthy eating habits, excessive alcohol consumption, lack of exercise and smoking.
What causes can osteoporosis have?
When asked about the causes of osteoporosis, many people want a clear reason – which could be nutrient deficiency, a drug or genetic predisposition. However, several causes of osteoporosis usually play a part.
What is primary or secondary osteoporosis?
Physicians differentiate between primary and secondary osteoporosis. Primary osteoporosis refers to when the disease has developed without an apparent cause. In contrast, secondary osteoporosis is caused by an underlying disease, such as a hormone disorder, hyperthyroidism or chronic gastrointestinal disease.
Certain factors in lifestyle, but also diseases or special medications, can contribute to the development of osteoporosis.
Nutrition & lifestyle:
- Lack of movement
- Genetic predisposition
- Low-calcium diet
- Vitamin D deficiency
- Excessive alcohol consumption
- Excessive nicotine consumption
- Oestrogen deficiency (e.g. menopause, late onset of puberty, removal of the ovaries)
- Chronic underweight, eating disorders
Certain diseases, such as:
- Gastrointestinal diseases (e.g. impaired nutrient utilisation, stomach reduction, chronic inflammatory bowel diseases)
- Rheumatic diseases
- Parathyroid gland hyperfunction
- Type 1 diabetes
- Renal insufficiency
- Pancreatic weakness
- Liver cirrhosis
Certain medications, such as:
- Glucocorticoids (cortisone)
- Antidepressants
- Proton pump inhibitors (stomach protection)
- Long-term heparin therapy
- Overdosed thyroid hormones
Prevention instead of therapy: How can osteoporosis be prevented?
Robust bones are a long-term project worth investing in – a balanced diet with a high percentage of fruits and vegetables, good year-round vitamin D supply and regular physical activity into old age form the basis for this. In addition, the following applies: Measures that help prevent osteoporosis are an important part of the therapy even in the case of pre-existing osteoporosis.
A diet to strengthen bones
A sufficient supply of nutrients that support the bones plays a significant role in creating strong bones both in our youth and as we get older. In addition to a high-energy, alkaline diet (rich in vegetables, herbs and fruit), optimum vitamin D levels should be ensured all year round – i.e. moderate sunbathing between April and October, a supplementary vitamin D intake for the rest of the year.
Important bone-relevant vitamins & minerals
Calcium: Calcium is good for the bones. Many of us had this drummed into us from primary school age. Although the mineral does not build up our bone structure alone, it is its most important structural component. Approximately 98% of total body calcium is located in the bone.
Vitamin D: For a long time, only calcium was associated with the bones by most people. However, thanks to years of educational work, many people are now aware of the importance of another bone nutrient, vitamin D. This fat-soluble vitamin is required to absorb calcium from the intestine and to integrate it into the bones.
Vitamin K: Many people are less aware that vitamin K is also important for healthy bones. This fat-soluble vitamin plays a role in activating bone formation.
Supplementation
Compound food supplements can provide our bones with the right micronutrients in a targeted and meaningful manner. Recommended preparations are based on the latest study findings. In addition to vitamin D, calcium and vitamin K2, less well-known bone nutrients such as magnesium, phosphorus, manganese, zinc and boron can also contribute to the strengthening of bones. However, in order to stimulate the mineralisation of the bone, another important measure must be present, namely...
...sports & strength training
Use it or lose it really does hold true. No more suitable proverb could be found in terms of bone health. Whether it’s jogging, skipping, tennis or hiking – sports that put pressure on our bones signal to our body that it is worth investing in bone mineralisation. And all age groups should realise that they are affected: At a young age, sufficient physical exercise improves the development of bone density and thus increases peak bone mass – the maximum value of bone mineral density in humans, as achieved by adults around 30 years of age with healthy bones. In advanced age, exercise and strength training reduce the rate of bone density loss.
Early bone density measurement
The right movement and bone-relevant nutrients are the ideal basis for strong bones. But do you know your own bone density? You can find this out with a simple bone density measurement.
Bone density normal values & osteoporosis values
The so-called T-value (also: T-score) is determined to assess bone density. This value indicates how much a person’s measured bone density differs from the bone density of same-sex young healthy adults (30 years old).
- Values that are higher or equal to -1 are considered normal here.
- With values between -1 and 2.5, this is called osteopenia (= an osteoporosis precursor).
- If the T-score is lower than -2.5, osteoporosis is present.

Can bone density be built up?
As active living tissue, the bone can renew itself for a lifetime, so even after reaching maximum bone density at about 30 years, it is possible to maintain bone degradation in a stable manner with the help of targeted measures (= a diet with bone-healthy micronutrients, healthy lifestyle and physical activity) – or even to achieve an improvement in bone density.
Conclusion: Osteoporosis is a silent killer, which can only be nailed down with a bone density measurement. If bone density is different from the norm, you should take action. In addition to a bone-friendly diet, special dietary supplements can target bone metabolism. Preparations that contain not only calcium, but also at least vitamin D and vitamin K are recommended. And of course, bone-encouraging exercise is also essential. Because “use it or lose it” applies even to the strongest.
FAQs
Bone density can be improved at any age. This requires hard training, a diet for healthy bones, sufficient vitamin D and a healthy lifestyle. In addition, a customised bone preparation can give additional support.
A T-value between 0 and -1 is known as normal bone density.
The following measures help to counteract osteoporosis: Regular physical exercise, a high-energy, alkaline diet and an optimal vitamin D level all year round. In addition, alcohol should only be consumed to a small extent and smoking should be avoided altogether.
References:
Berufsverband Deutscher Internistinnen und Internisten. 2023. https://www.internisten-im-netz.de/krankheiten/osteoporose/ursachen/, Zugriff:
Garach A.M. et. Al 2020. Nutrients and Dietary Patterns Related to Osteoporosis Nutrients. 2020 Jul 3;12(7):1986. doi: 10.3390/nu12071986.
Papadopoulou S.K., et al. 2021. Exercise and Nutrition Impact on Osteoporosis and Sarcopenia-The Incidence of Osteosarcopenia: A Narrative Review. Nutrients. 2021 Dec 16;13(12):4499. doi: 10.3390/nu13124499.
Capozzi A., et al. 2020. Calcium, vitamin D, vitamin K2, and magnesium supplementation and skeletal health Maturitas. 2020 Oct;140:55-63. doi: 10.1016/j.maturitas.2020.05.020. Epub 2020 May 30.
Fusaro M., et al. 2020. Vitamin K and Osteoporosis. Nutrients. 2020 Nov 25;12(12):3625. doi: 10.3390/nu12123625.
Ma M.-L., 2022. Efficacy of vitamin K2 in the prevention and treatment of postmenopausal osteoporosis: A systematic review and meta-analysis of randomized controlled trials. Front Public Health. 2022 Aug 11;10:979649. doi: 10.3389/fpubh.2022.979649. eCollection 2022.
McCloskey, E. 2011. Preventing osteoporotic fractures in older people. Practitioner. 255(1736):19-22, 2-3.
Gröber, U. 2006. Osteoporose – Risikomanagement mit Vitalstoffen. Zs f Orthomol Med. 1:6-12.
Gröber, U. Orthomolekulare Medizin: Ein Leitfaden für Apotheker und Ärzte, 3. unveränderte Auflage. Stuttgart: Wissenschaftliche Verlagsgesellschaft Stuttgart, 2008.
Aktion Gesunde Knochen (ein Projekt der Österreichischen Gesellschaft für Gesundheit), 2023. https://www.aktiongesundeknochen.at/osteoporose-rund-um-die-welt-europa/, Zugriff:
DocCheck Flexikon, 2023. https://flexikon.doccheck.com/de/Juvenile_Osteoporose, Zugriff:
Resch J. 2019. Mit Biogena Osteo Calbon Komplex Gold die Knochenstruktur stärken. BIOGENA unver. Pilotstudie, 2019.